Coronavirus: Inside test-and-trace - how the 'world beater' went wrong

Exactly six months after Boris Johnson promised a "world beating" contact tracing system, it can be shown that the network is failing in areas with some of the highest infection rates.
The research also found no-one from NHS labs was at a key government meeting with private firms about testing.
The government has yet to comment.
As ministers struggle to get the test-and-trace system on track, BBC News spoke to key government figures, scientists and health officials who were involved from the very start to establish what went wrong with the system - and, crucially, whether the system can be fixed to hold the virus in check until vaccines come to the rescue. The investigation found a system that is failing in the areas where it is needed the most and is still undermined by the legacy of decisions they were made at the outset.
Further revelations include:
- Private contractors overpromised what they could do, with one saying it would build 200 testing machines that hadn't, at the time, even made it to prototype
- The move to more local contact tracing by councils was being undermined by IT problems, leading to a reliance on spreadsheets and delays getting contact details.
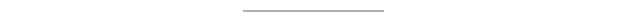
The name NHS Test and Trace sounds like it is one whole service that is part of the NHS. Nothing could be further from the truth.
It is a complex web of different programmes that have been bolted together rapidly. Private firms play a key role in terms of both testing and tracing, which has meant some of the local expertise available in the NHS, universities and councils has been bypassed.
The seeds for this were sown back on 17 March before the first lockdown was announced when a group of companies met with government to discuss testing.
That meeting included now-key players Randox and ThermoFisher, two health-technology firms. But no representatives speaking for the existing NHS labs sector were involved, says Allan Wilson, president of the Institute of Biomedical Science. "There wasn't any consultation with the service itself."
Very quickly the direction of travel became clear - the government turned to its commercial partners to set up large, centralised labs that sat outside any existing healthcare or research structures.
There is now a network of six large mega-labs - known as Lighthouse labs - that process the bulk of the tests across the UK. Testing sites, where the swabs are taken, are run by the auditors, Deloitte.
A similar decision was made with contact tracing - a national army of 18,000 contact tracers taken on by outsourcing company Serco, while Sitel runs the contact centre. This element just covers England. The rest of the UK has its own arrangements.
"These contracts were signed and sealed in record time - there weren't even penalty clauses inserted for performance in many," says someone who was close to the decision-making at the time. "The government was in a panic - we were in the middle of lockdown and they were under pressure from all angles. It is not the environment in which the best decisions are made."
And so it proved.
The centralised system that bypassed local skills
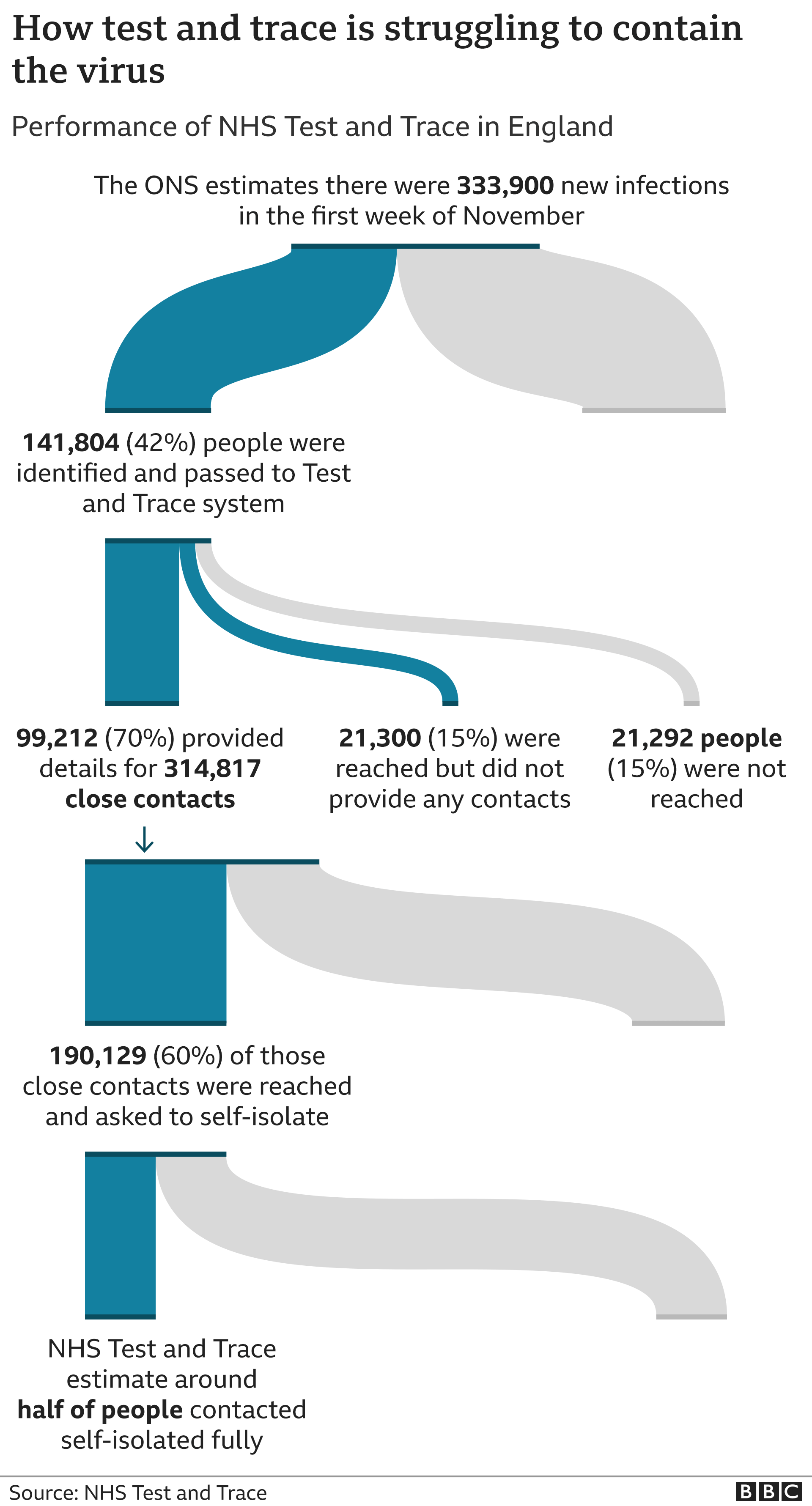
The government has now got a large testing capacity - it can process more than 500,000 virus tests a day. At the start, the UK could only do 2,000. But the system has struggled to shorten the time it takes from someone being swabbed to getting a result.
"If we'd kept it local we would have been able to turn those tests around much quicker," says Mr Wilson, referring to the existing network of hospital, university and Public Health England labs. "We already had the logistics in place."
Instead, an entirely new system had to be set up to get the samples into the Lighthouse labs, with swabs travelling long distances - sometimes by plane from Edinburgh to Belfast - slowing down the process to this day.
Dr Rachael Liebmann, vice-chair at the Royal College of Pathologists, who works in both private and NHS labs, says: "The default was to go outside the NHS for something new and shiny. But there was not enough input from people who understood testing."
According to Allan Wilson, the government was "speaking directly to the commercial companies and saying - what can you do for us?" There was no voice of challenge, "saying 'that won't work'".
Randox - which won almost £500m of contracts from the Department of Health - planned to recruit 200 new staff to help ramp-up Covid-19 testing. It said the company would be building 200 testing machines over the following six weeks. At this stage, though, its makers had not yet completed a single finished prototype of the machine, and had previously expected they would ultimately be able to build about 10 a year, the BBC understands. By September, not a single machine had been finished. The staff that were recruited to build them would often be sent home or were left sitting around.
A Randox spokesperson said the firm had "not only met but exceeded all government programme expectations. In fact, Randox processes more samples than any other laboratory in the UK."
Meanwhile, other companies were selling testing machines to NHS-run labs which did testing for hospitals. This was despite the fact the kits and chemicals needed for those machines were in short supply and being snapped up by the privately-run Lighthouse labs.
"There are labs that bought... equipment and still are not able to run them at capacity due to a lack of reagents [chemicals needed for testing]," Dr Liebmann says.
Hitting the target but missing the point?
The government's obsession with hitting testing targets has also been heavily criticised. First 10,000 tests a day by the end of March, then 100,000 a day by the end of April, before a target for capacity of 500,000 a day by the end of October. But there was less focus about who should get those tests and why.
Despite regular advice to do so, people working in hospitals were not screened for coronavirus unless they had symptoms. This has only just started happening, despite evidence showing significant transmission in hospitals. But there were labs that did set up regular screening for healthcare staff of their own accord - despite being "effectively discouraged" to do so, according to one source.
The University of Cambridge was one example, its research lab partnering with nearby Addenbrooke's to offer screening to its hospital staff at the peak of the UK epidemic's first wave. By the end of June it had screened more than 10,000 people working in the hospital, to detect asymptomatic carriers, says Dr Stephen Baker, who was involved in creating the programme.
"It had a really big impact on keeping the hospital going," and, he believes, helped give NHS staff some sense of safety and morale.
September - the moment testing fell over
Many of the issues with testing played out behind the scenes. But they came under acute public scrutiny in September when tests became near-impossible to access - just at the moment the second wave was taking off.
Part of this was driven by individuals applying for tests on return from holidays, and children going back to school. But there were also issues of capacity in the labs themselves. One volunteer in a Lighthouse lab, a virologist who wanted to remain anonymous, told the BBC supply chain issues slowed progress: "We would never know how many samples were going to come in. We had a forecast each day but they were never right."
This meant sometimes having enough staff to process 10,000 samples and only receiving 2,000, leaving people sitting around, and on other occasions receiving many more than expected and struggling to deal with them.
While scientists were involved in setting up the labs, they weren't necessarily people "who had any idea how to deal with viruses", meaning "procedures were constantly tweaked" and there were issues with recruitment and training which again slowed things down.
Why tracers have to make multiple calls to families
Testing is one part of the equation for containing coronavirus. Every bit as important is the ability to trace close contacts of those infected, ensuring they isolate at home. For the tracing service, which went live at the end of May, just a week after the prime minister's world beating promise, problems have played out in different ways.
It causes a massive amount of stress - a lot of contact workers are upset because they get a lot of abuse about it
About 18,000 contact tracers were hired - only about 3,000 of them came from a clinical background.
That in itself was not necessarily an issue. Those involved in the service say the people who get the best results are the good communicators. The problem is that so often the centralised call centre-based approach did not let them communicate. Contact tracers were told to follow heavily scripted cues.
There was no room for discretion. It has led to the situation whereby call handlers have to try to make individual calls to every member of a household and go through the same forms. This is part of the reason some families have found themselves receiving lots of calls. It is in the process of being scrapped.
One test-and-trace manager told the BBC it has undermined the system throughout. "It causes a massive amount of stress. A lot of contact workers are upset because they get a lot of abuse about it."
Failing in the areas that need it the most
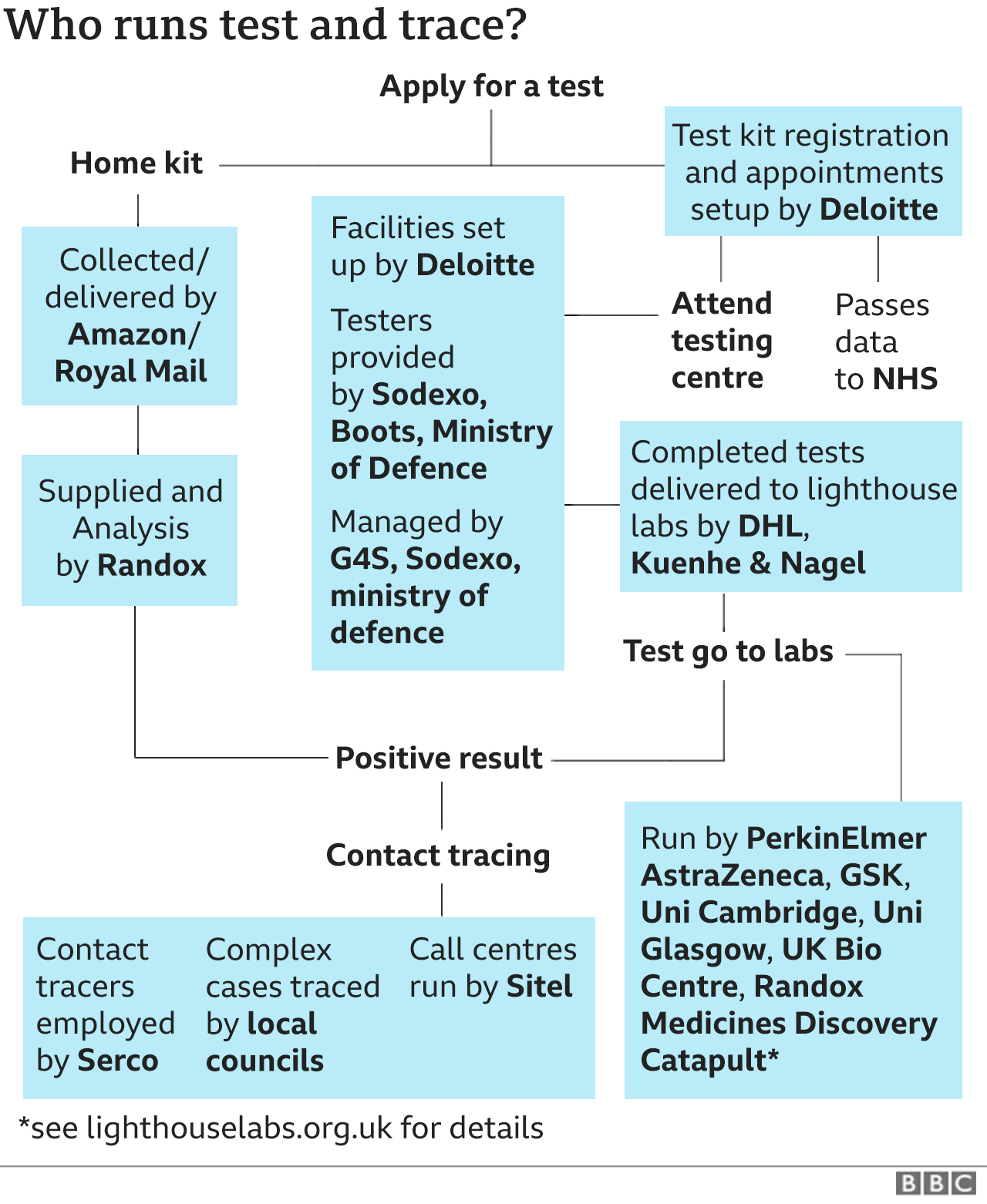
Overall, performance has fallen short of what was hoped for. To be effective, government advisers say 80% of people who test positive should be reached and details of their close contacts - chiefly family, friends and work colleagues - obtained. Then 80% of those contacts ought to be reached and asked to isolate. In some areas just half of close contacts are being reached and asked to isolate. A number are in the areas with the highest rates, such as Bradford, Manchester, Luton, Blackburn and Nottingham.
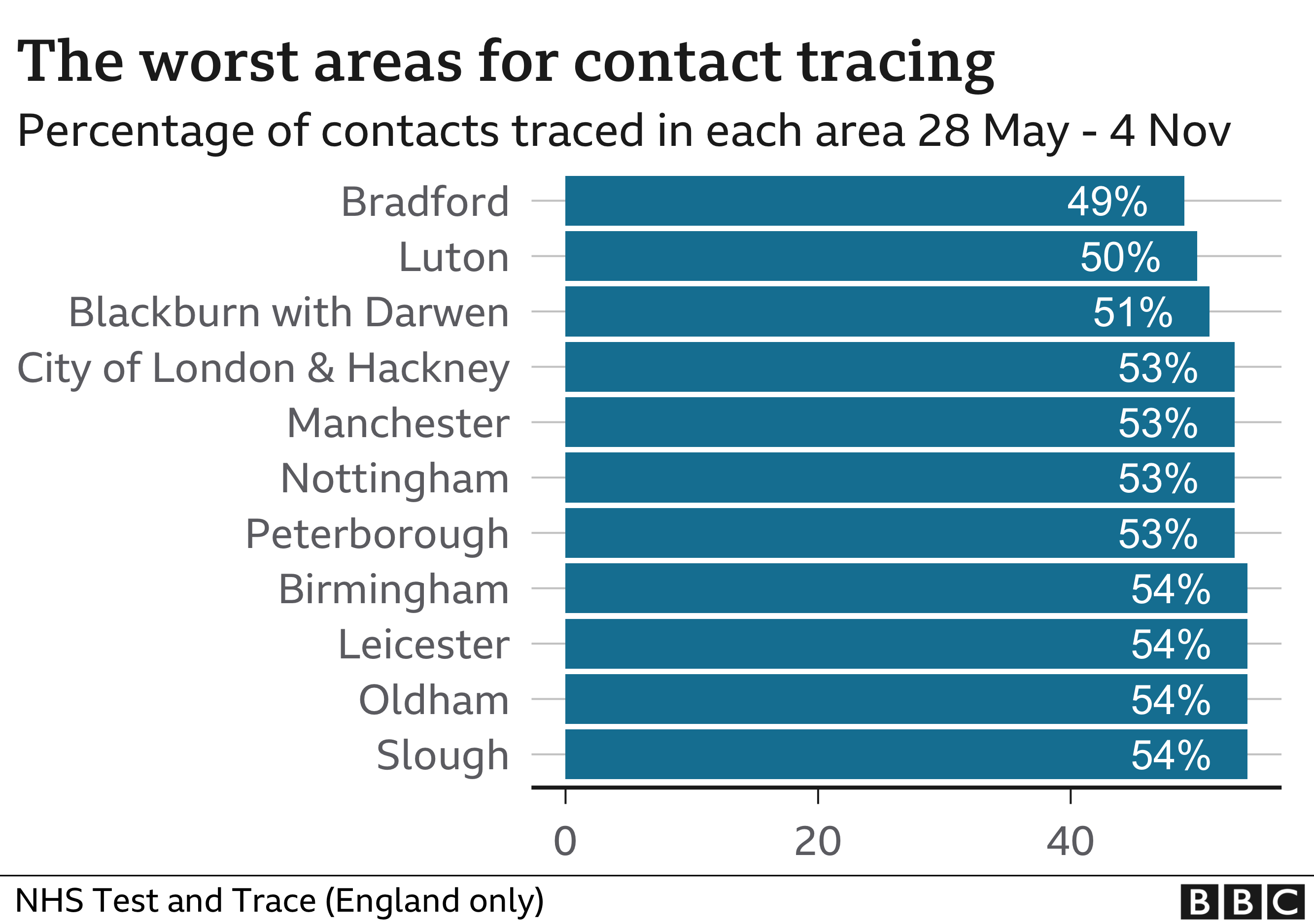
The targets are rather broad brush. For one thing they ignore the fact that the testing system is routinely failing to identify about half of cases. The blame for this cannot be laid solely on the government - with so many infected people not showing symptoms, the system is up against it from the start. But with the targets missed almost every week, it quickly became clear there was too much focus on the national system and not enough on local.
Has Dido Harding being unfairly maligned?
Much of the criticism has been aimed at Baroness Dido Harding, who was recruited to head up NHS Test and Trace. However, this was only once the contracts had been signed and the model of working established. Working with what she has, she is adamant her team have performed well, regularly pointing out that despite the problems the service is still doing better than those in many other countries.
She says a system as "complex as Tesco" with its network of stores, distribution centres and supply chains has been built in a matter of months.
You can't expect test-and-trace on its own to keep on top of the virus
"It will keep improving," she says. "But you can't expect test-and-trace on its own to keep on top of the virus - it is just one part of a wider approach."
Comparing performance globally is difficult. Many do not publish the detailed information that England's service does. Even the data provided in the rest of UK is more limited by comparison - although it suggests those systems have struggled too. But some countries have fared better - Germany and South Korea, for example. The Health Foundation says the key is those countries' greater emphasis on local teams.
Local councils 'given hospital pass'
The need for greater local involvement was actually recognised by the government back in the summer. On 10 August, ministers announced they were changing tack and the national contact tracing team would be cut by 6,000. Staff were to be made available to councils to allow them to set up local teams which could take on responsibility for tracing cases after the first 24 hours. It followed the success seen in a small handful of areas that had decided to set up their own local contact tracing teams.
The announcement by government was widely welcomed by directors of public health, but then nothing happened. It was not until late October that ministers came up with an extra £1bn for the winter. This has been a source of huge frustration. Councils had been calling for more involvement from the start.
And as local schemes have got going - over a half have services up-and-running now - they have faced difficulties because of the centralised nature of the system. Among the problems reported are:
- Delays getting cases passed down from the national team
- Cases that are passed on are missing key contact information or are duplicates of cases already traced, wasting valuable time
- Lack of access to the central IT system used by NHS Test and Trace, meaning councils are having to record the information they collect on spreadsheets
- Councils are only allowed to trace the infected case - leaving them powerless to deal with family members, for example, even if they are on the door-step
"It's a complete nightmare," says one public health consultant who has set up a service. "We've been given a hospital pass. They never thought about using the local teams so the infrastructure isn't there."
Isolation - the forgotten part of the test-and-trace system
While £10bn was set aside for test-and-trace to help them find individuals, it seems very little thought was given to how people should be supported to isolate. The number isolating both after a positive test or because they are a close contact, is not routinely measured. Some research has suggested it may be as low as one in five, but NHS Test and Trace has put the figure at close to half. Either way, it is a glaring issue. A few have argued the isolation period is too long.
Some other countries only require seven days' isolation for close contacts, says Prof Tim Spector, who runs the popular C-19 symptom tracker app. "More reality and pragmatism is now needed to keep people on-side," he says.
On top that, there are questions about financial support for people who can't work while isolating at home. Until late September there was none beyond statutory sick pay. Now there is a one-off £500 payment for people on benefits. People who are asked to isolate via the app are not even entitled to this. Contact tracers the BBC spoke to say this is causing problems. "When we do get through, people are often uncooperative. They have lives to get on with and work they have to do to get paid."
Prof Robert West, from University College London's public health department, believes this is one of the most important issues with the whole system.
"We need to do much more to help - then we can create strong social norms that it would be unthinkable to violate."
The problem, though, he says, is we have missed the boat. With infections high, the window for getting this right has gone. "If introducing lockdown late was our biggest mistake in the first wave, in the second it is the fact we wasted the time that lockdown bought us to get an effective test-and-trace system running."
Have you been affected by the issues raised in this story? Tell us by emailing haveyoursay@bbc.co.uk.
Please include a contact number if you are willing to speak to a BBC journalist. You can also get in touch in the following ways:
- WhatsApp: +44 7756 165803
- Tweet: @BBC_HaveYourSay
- Please read our terms & conditions and privacy policy
If you are reading this page and can't see the form you will need to visit the mobile version of the BBC website to submit your question or comment or you can email us at HaveYourSay@bbc.co.uk. Please include your name, age and location with any submission.

November 20, 2020 at 01:00PM
https://www.bbc.co.uk/news/health-55008133
Labels: BBC News

0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home